Menstruation and T1D
If you have type 1 diabetes (T1D), menstrual cycles can affect your diabetes management. Your blood glucose may rise higher or lower than usual, and you may be more resistant or sensitive to insulin during your cycle. Everybody is different.

How do periods affect type 1 diabetes?
Before and during your period, your body may respond differently to insulin. You may experience high and low blood glucose levels before and during your period.
If you can determine what pattern your body follows in the run up to and during your period, it can help you better manage these changes.
The important thing to note is that menstrual cycles are very different for everyone. There is no one size fits all, and your own patterns can change throughout your menstrual years.
How do periods affect insulin?
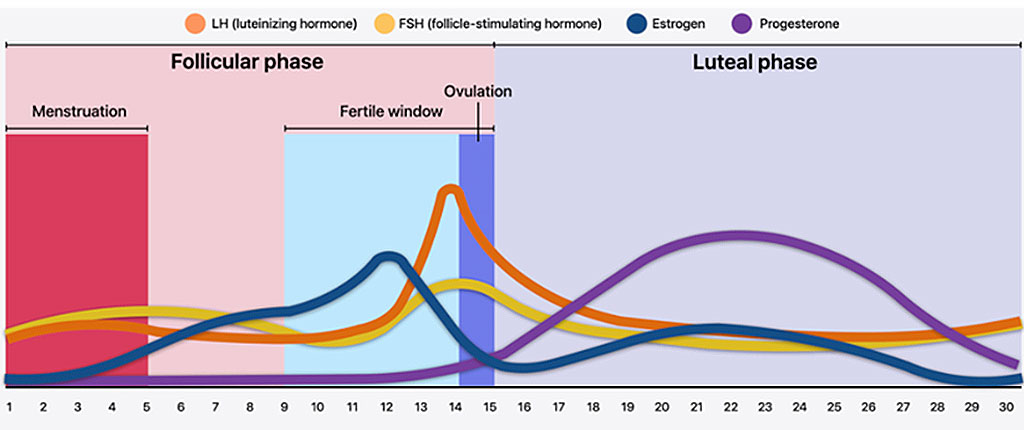
Your hormonal cycle – when estrogen and progesterone levels rise and fall – is broken up into two phases: a follicular phase and a luteal phase.
During the luteal phase (10-14 days before a period), progesterone levels are higher which can cause insulin resistance for some people.
When progesterone levels are higher, this can trigger cravings for things like chocolate, sugary foods, and white bread. It can cause tiredness too, making it harder to exercise, which can also increase insulin resistance.
Once you enter the follicular phase and your period starts, your insulin may suddenly seem like super-strength insulin. So, you may swing from high to low blood glucose levels which can be challenging. In fact, some women find that they need less insulin during this phase.
How do periods affect blood glucose levels?
During the lead-up to a period, blood glucose levels tend to run higher than normal. During a period, glucose levels can be lower than normal. But for some people it can be the opposite. Others don’t notice an effect at all. And for some, it can change from month to month.
Checking blood glucose levels more frequently before, during and just after a period can help you to work out what your pattern is during your menstrual cycle. Technology, such as advanced glucose monitors like continuous glucose monitors (CGM) and flash glucose monitors (Flash GM), can help you to make informed decisions about adjusting your insulin and the carbohydrates you’re eating to try and minimize the chances of experience hypoglycemic episodes.
Can insulin affect your period?
Insulin itself doesn’t have a direct impact on your period.
Can type 1 diabetes cause heavy periods?
If you spend 70% or more in the optimal glucose range (usually 4-10 mmol/l), you may have a more stable menstrual period pattern (you can find out your time in range percentage on your CGM or flash glucose monitor). Genetics also have an influence, so what is ‘normal’ for one person with a 70% time in range will be different from others.
Spending a lot of time outside your target range probably means that there will be changes from month to month (depending on your cycle) and this could include heavier or missed periods. This is because extreme changes in glucose levels impact how your hormones work.
Some months, you may experience heavy bleeding, other months your cycle may be lighter. The heavier your cycle, the higher your insulin needs may be.
Can type 1 diabetes cause periods to stop or become irregular?
When you have T1D, you may experience irregular or unpredictable menstrual cycles. Keeping your glucose levels in target range 70% of the time will mean there is less impact on the hormones regulating your menstrual cycle.
It isn’t always possible to keep your blood glucose consistent. Things like stress or illness, or even changes in the weather can make it harder to manage your blood glucose. These normal life events can cause your usual menstrual pattern to change.
Talk to your diabetes healthcare team if you aren’t having periods at predictable intervals or need support to manage your blood glucose.
Make the most of diabetes technology
Keeping a menstrual diary alongside your blood glucose data will help you work out your pattern. Advanced glucose monitors allow you to take notes so that you can look back over the logbooks and match your blood glucose data against your period.
Because it’s constantly recording, a glucose monitoring system makes it much easier to see what’s going on in terms of how your insulin is working and what your glucose levels are doing. It might help you to know for example whether you’re particularly insulin-resistant a few days before you’re due to start your period.
What about diabetic ketoacidosis (DKA) and the menstrual cycle?
If you become very insulin-resistant in the lead-up to a period and if your insulin dose is not adjusted, you may not have enough insulin in your system to break down carbs effectively to use as energy.
This can lead to a higher blood glucose level and may cause ketones to build up in the body. Ketones build up when there is not enough insulin in the body to convert glucose to energy, so your body starts breaking down fat instead. Too many ketones can lead to diabetic ketoacidosis (DKA), which can be life-threatening if it is not treated quickly. It can also have an effect on ovulation and fertility.
If you are concerned about ketones, you can monitor your ketone level using a blood ketone monitor.
Can diet and exercise help with period symptoms?
Good nutrition, exercise and regular sleep are ideal goals for everyone, whether they have type 1 diabetes or not. Hormonal changes can make you feel hungrier which may cause cravings for sugary food before your period.
Eating healthier carbs when possible may help to keep blood glucose levels more stable. If you’re able to exercise, finding a type of exercise that works for you may also help you better manage period symptoms.
Get support
Talk to your support network, and in particular family members who menstruate to get an idea of what their menstrual cycle is like. Connecting with other people who live with T1D through online communities and forums can also be helpful.
Share any concerns about managing your blood glucose alongside your periods with your diabetes care team or your primary care physician. You could also ask about options for controlling the hormonal shifts that happen during the menstrual cycle.
*content taken from Breakthrough T1D UK and revised for the Canadian type 1 diabetes community