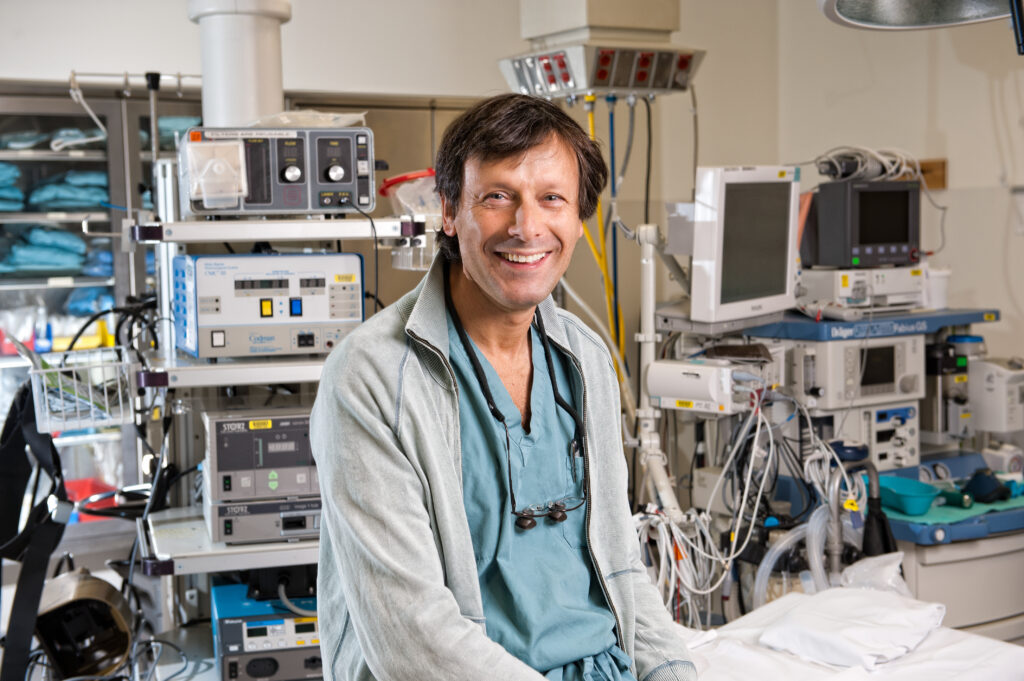
Dr. James Shapiro is a British-Canadian surgeon best known for leading the clinical team that developed the Edmonton Protocol – an islet transplant procedure for the treatment of type 1 diabetes (T1D). Dr. Shapiro is Professor of Surgery, Medicine, and Surgical Oncology at the University of Alberta and the Director of the Clinical Islet Transplant Program and the Living Donor Liver Transplant Program with Alberta Health Services. He holds a Tier 1 Canada Research Chair in Regenerative Medicine and Transplantation Surgery.
Dr. Shapiro obtained his medical degree from the University of Newcastle upon Tyne and trained in surgery at the University of Bristol. After coming to Canada in 1993, he received training in liver transplantation and hepatobiliary surgery at the University of Alberta and earned a PhD in Experimental Surgery.
Shapiro developed a brand-new approach to optimize islet cell transplant engraftment. Of almost 300 islet transplants attempted before 1999, fewer than 10% of these worked in patients. His protocol was designed to address many of the previous shortcomings by transplanting a sufficient number of islets into the liver by using multiple donors, and by testing a novel anti-rejection strategy that avoided steroids as immunosuppression to allow the transplanted islets to work at their best. The result became known internationally as the ‘Edmonton Protocol.’
Shapiro led the clinical team that tested his approach in seven initial patients, all of whom (100%) were able to discontinue the need for insulin injections for periods beyond a year. He was the lead author in the landmark paper published in July 2000 in the New England Journal of Medicine detailing the results of the Edmonton Protocol.
In the 24 years since, Dr. Shapiro and his team have performed this transplant 765 times in over 300 Canadians and continue to refine and optimize the protocol. This treatment has been replicated many times internationally, and over 2000 patients worldwide have now received islet transplants from the foundations developed by the Edmonton Protocol.
JDRF Canada recently spoke with Dr. Shapiro about the future of cure-based T1D research as they commemorate 50 years of the organization.
JDRF Canada: What excites you most about stem cell therapy as a potential cure-based therapy for type 1 diabetes?
Dr. Shapiro – Diabetes is a biological disease. Insulin injected into the fat below the skin is a chemical but imprecise way of controlling the disease. By replacing the beta cells in the pancreas that are killed or not functioning well, cellular transplantation provides an elegant biological solution to control this biological disease. I am particularly excited about stem cells for the potential to cure not just T1D, but all types of diabetes. Injected insulin is life saving in the short term, but the subcutaneous fat is a weak link in the chain, failing to provide perfect glucose control. Stem cell-based treatments have the potential to function in a way that most closely resembles the process of insulin release and control that happens from moment to moment inside the normal healthy body.
However, as of right now, powerful anti-rejection drugs are required for cell transplants to survive, and these drugs carry potentially risky side effects. So, this means it’s not currently a good option for children and for many adults. How could we circumvent a need for these drugs with stem-cell-based islet transplants, and make the treatment safer and more available for all?
This can be achieved either by altering the cells themselves to help them evade immune attack, or it can be done by different kinds of approaches that induce something called immunologic tolerance, but this has proven in the past to be a tough nut to track.
I’m most excited about the potential to make personalized cells, using an individual’s own cells to work as treatment. This is the biologically closest option from a concept perspective, albeit the hardest from a manufacturing standpoint using today’s methodologies – but this will change and become much simpler over time. We need to still deal with autoimmunity in T1D, but this can be potentially achieved either through biologic drugs, or far milder gene editing.
I’m very excited about the progress of T1D research, especially within the last five years. But I believe that a cure is really within all our grasps. It’s going to require intense collaborative scientific effort and a lot of funding, but I firmly believe this is possible and will happen.
The Edmonton Protocol, which was pioneered by you and your team, is considered the first step on a path to a stem-cell based cure for T1D. How did you feel when it was shown that islet cell transplants could be successful in helping to treat patients with uncontrolled T1D?
To be honest, the first Edmonton Protocol patient we transplanted – a teacher from Yellowknife, I didn’t feel particularly excited. You have to remember that there had been nearly 300 attempts before, and very few worked. His first transplant brought his insulin down by half. We decided to give him a second transplant and he came off insulin entirely.
It was my first year of practice as a busy transplant and liver surgeon, and we started two new programs that year (pancreas transplant and living donor liver), and I really didn’t believe that cell transplants would work. It was only when the 7th patient was treated and all seven were insulin free that I was pretty excited. Clearly, we had something different, something that was clearly working, something that was reproduceable. It was a delayed excitement however, and it was an exercise in patience getting the paper out in the New England Journal of Medicine (it required lots of revisions, they kept asking for further data etc.), but finally it really re-invigorated the field, both in islet cells and the future of stem cell therapy.
Other than stem cell research, what other area of T1D research do you find holds the most potential for a cure?
Preventing T1D at the outset in children and adults at highest risk would have the biggest future impact, avoiding need for transplants. Preventing autoimmunity in the beginning stages and combining that with islet cell differentiation techniques learned from all the work with stem cell research could be applied early enough to prevent T1D from occurring. If we can induce cellular regeneration in the pancreas in the native islets along with stopping autoimmunity, that would be an elegant solution to reduce new cases of T1D. The challenge is doing this without inducing pancreatitis and other risks to the organ. Treating patients and preventing the disease will be an incredibly important next step.
In terms of type 2 diabetes, the newer drugs like Wegovy and Ozempic, these GLP-1 agonist medications are really making inroads, and this will be a game-changer for this disease to reverse or treat before it can become life-threatening.
Stem cell therapy is tantalizingly close, which is why I can’t stop thinking about it day and night. But I see new frontiers every day in the treatment of all types of diabetes.
Things are looking bright, but they never happen quite as fast as we want them to as scientists, and certainly not as fast as children and their desperate parents need. We need new ideas, new resources and new partnerships to make it happen. And I firmly believe our partnership with JDRF Canada is going to make that happen.
What role do you see JDRF Canada playing in the next (hopefully less than) 50 years when it comes to T1D cures research?
Because we are so tantalizingly close, an immense amount of intensive, focused translational research needs to be done. The potential to make autologous islet cells (made from your own blood cells), is an ambitious, challenging and expensive approach, and to move this forward we will need both philanthropic and industrial support to get to the next stage. I can’t stop thinking about that next set of seven patients, all of whom will be off insulin – but with no need for antirejection drugs. This will happen with JDRF, their connections to philanthropy and ability to move grants rapidly through to the researchers that will get this job done.
I am incredibly grateful to JDRF for their support, for enabling the work that led to the Edmonton Protocol and moving the field forward since then. JDRF has been phenomenally powerful as an advocate, with governments, with patients; it’s been a wonderful partnership that will need to continue to get us across the finish line.