The American Diabetes Association’s 84th Scientific Sessions were held from June 21- 24th 2024. This annual conference brings together researchers and scientists to both present and learn about the latest in type 1 diabetes research and technological advancements. Many of the presentations features study results from researchers funded by Breakthrough T1D (formerly JDRF International) and JDRF Canada. The work presented at ADA will advance research and ultimately improve outcomes for people with diabetes (T1D).
Updates in Cell Therapy Research:
Cell therapy aims to replace the insulin-producing beta cells that are destroyed in people with type 1 diabetes so that they can produce their own insulin again.
Vertex Pharmaceuticals presented an update on their VX-880 product, a stem cell-derived replacement therapy with immunosuppression. Of the 12 patients who have been dosed, nearly all (11 of 12) have has a reduction or elimination of exogenous insulin use (via pump or injection). All patients have achieved an HbA1C below 7.0% and time-in-range above 70% on continuous glucose monitoring with the reduced or eliminated insulin administration. There have been no serious adverse events reported. The trial is expanding recruitment for 37 participants to progress towards pivotal development.
This research was made possible by years of funding by JDRF and the T1D Fund to Doug Melton, Ph.D., and Semma Therapeutics—a biotech company founded by Melton to develop a stem cell-derived islet therapy for T1D—which was acquired by Vertex Pharmaceuticals in 2019.
Cristina Nostro, University Health Network, presented an overview on her JDRF-funded work designing an optimal beta cell surrogate. Her work ranges from establishing optimized stem cell products to the use of microvessels for the purpose of increasing cell engraftment after transplantation.
Alice Tomei, University of Miami and Diabetes Research Institute is funded by Breakthrough T1D (formerly JDRF International) to examine immune protection strategies for immune protection of transplanted beta cells. She presented an update on research that looks to co-deliver immunomodulators via biomaterials along with transplanted beta cells to provide local, specific immune protection.
Jeffrey Millman, Washington University, presented work on his research looking into making stem cell-derived beta cells more functional so that they produce insulin levels similar to healthy human beta cells. To date, stem cell-derived beta cells have underperformed compared to healthy human beta cells.
Katy Digovich from Minutia presented ongoing research funded by an Industry Discovery & Development Partnership grant from Breakthrough T1D. They are developing nanoparticle trackers that provide real-time monitoring to assess and modify beta cell transplant health post-engraftment in patients with T1D.
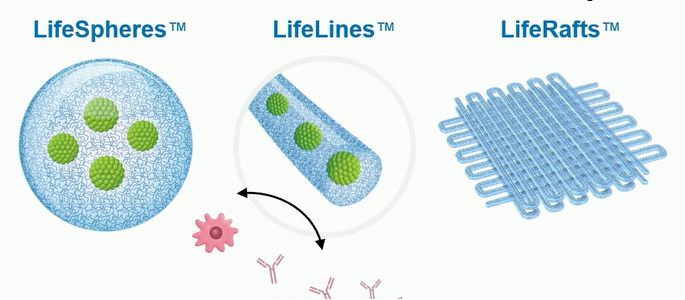
Harald Stover from Allarta Life Science (Hamilton, ON) presented ongoing research funded by an Industry Discovery & Development Partnership grant from Breakthrough T1D. Their work focuses on synthetic gel coatings that are designed to both support (with nutrients and oxygen transfer) and protect (with immune evasion) beta cells during transplantation.
Updates in Disease Modifying Therapy Research
Kevan Herold, M.D., presented a secondary analysis of the phase III PROTECT clinical trial. In October 2023, Tzield™ (teplizumab-mzwv) showed that it can slow the loss of beta cells and preserve beta cell function in newly diagnosed (stage 3 T1D) children and adolescents ages 8-17. This analysis demonstrated that, in addition to slowing down the loss of beta cells in new-onset T1D, Tzield can decrease insulin dose and improve time-in-range. This reinforces our commitment to supporting therapies that preserve beta cells at onset, which is important for the prevention of complications and improvement in new-onset clinical factors.
Learn more: https://www.breakthrought1d.org/news-and-updates/ada-takeaways-day-1/
Updates in Screening and Monitoring of Early Stage T1D:
Breakthrough T1D spearheaded an effort to develop the first internationally agreed-upon guidance for anyone who tests positive for T1D autoantibodies, co-published in the journals Diabetes Care and Diabetologia.
These provide guidelines for monitoring children, adolescents, and adults who test positive for T1D autoantibodies, along with recommended monitoring frequencies and actions for healthcare professionals when the risk of progression toward symptomatic T1D is high.
The guidance also includes recommendations for educational and psychosocial support for positive T1D antibody individuals, including their families and caregivers, and may also lead to primary care doctors screening more frequently since there is actionable monitoring guidance available to them.
For the first time, individuals, families, and healthcare professionals have concrete next steps to monitor early stage T1D progression and catch symptoms early to prevent DKA.
This guidance was developed with over 60 international experts, representing 10 countries and endorsed by 11 national and international societies.
The author list includes Dr. Diane Wherrett of SickKids Hospital, lead of the JDRF-CIHR funded CanScreenT1D Canadian Screening Research Consortium https://breakthrought1d.ca/canscreent1d-screening-research-consortium-in-canada-announced/
Updates in T1D Devices:
- Medtronic MiniMed 780G, especially the importance of initiating it as soon as possible following diagnosis (which is now recommended in the ADA Standards of Care for both children and adults), citing the CLVer trial, which found clinically meaningful and sustained improvements in blood sugar management following early AID initiation.
- Medtronic MiniMed 780G in high-risk youth with T1D, with 80 participants aged 7-25 years, who demonstrated an average HbA1c reduction of 2.5% (from an average baseline HbA1c of 10.5% to 8%), improvement in time-in-range, and a reduction in low blood sugar events.
Learn more: https://www.breakthrought1d.org/news-and-updates/ada-takeaways-day-2/
Updates in T1D Complications
SGLT2i Shown as Potential Solution to Help Manage Renal Complications and Improve Glycemic Control for Young Individuals Living with Type 1 Diabetes
Findings from Dr. Farid Mahmud’s JDRF funded ATTEMPT study, showed that a low-dose of SGLT2 inhibitor could safely be given to youth and adolescents with type 1 diabetes (T1D) to improve kidney function and glycemic management. ATTEMPT is the first of its kind, landmark trial designed to evaluate the effectiveness of SGLT2 inhibitors to optimize diabetes control and prevent early subclinical kidney complications in an at-risk pediatric population with T1D.
This medication was evaluated alongside safety protocols to mitigate the risk for diabetes ketoacidosis. It is not approved for T1D by Health Canada.
To learn more: https://ow.ly/FYuL50SoFxT
Updates in Psychosocial Aspects of Living with T1D
BETTER presentation
Maya Nehme, RD/Dt.P, Research Center CHUM presented results from a cross-sectional study that explored Diabetes Distress among Persons Living with Latent Autoimmune Diabetes of Adults in the Canadian Cohort BETTER. Initially funded through the JDRF-CIHR Partnership to End Diabetes, JDRF Canada has extended funding for the BETTER project for an additional 3 years.
The BETTER project includes a Canadian registry of people living with T1D, called the BETTER registry, in which people living with T1D (or LADA for Latent Autoimmune Diabetes in Adults) – or who have a child living with T1D – can share their experience through online questionnaires in order to enrich research and knowledge about T1D.
The study found that emotional burden is significantly greater in persons with LADA than in persons with type 1 diabetes. JDRF Canada is pleased to continue to support the BETTER project and enable such studies to shed light on the daily challenges of those living with T1D.