Mental health and T1D
Type 1 diabetes (T1D) is a chronic condition requiring daily management, which may affect you or your family’s emotional and mental well-being.

Each day can bring its own challenges, but finding the support you need can make all the difference.
“Living with type 1 diabetes is 24/7. There are no breaks, and it can be exhausting.”
– Alison, age 51, parent of teenager living with T1D
Immediate assistance
If you are in immediate danger, please call 911 or go to your local emergency department.
If you are in crisis, you can connect with responders here or at 1-833-456-4566
Diabetes stress management: developing resilience
Living with type 1 diabetes (T1D) isn’t always easy. You may experience stress from your demanding management routine, the cost of diabetes supplies and/or the perceived stigma of having a chronic condition.
The social and emotional effects of T1D are very real, and can lead to experiencing burnout, depression and anxiety. Despite these frustrations and hurdles, many people with diabetes are able to achieve positive outcomes in both their diabetes management and their personal lives.
The ability to overcome these challenges and rebound from low points is often referred to as resilience.
“Resiliency in diabetes is to hold onto our sense of normalcy, adventure, love and wonderment for the world all the while managing an ever present disease” – Laura, age 37, living with T1D
For some people, knowledge is power. By learning more about T1D, how to manage it, and the impact on you and your life, you can become better at predicting and managing different situations that may generate stress. For others, preparation and planning for different scenarios can help to reduce potential unknowns and stressors. A change in routine, like travelling, can be stressful. However, careful planning ahead can minimize stress. Even then – sometimes you can do everything “perfectly” and diabetes still doesn’t cooperate. This happens to everyone once in a while, but fostering resilience can help you realize that maybe it’s just a bad day, and to try again tomorrow.
How to build resilience
Everyone has personal strengths that they can identify and work on to try and become more resilient.
For example, someone who is highly organized might channel that trait into a more structured approach to coping and management. That could involve setting goals and planning ahead. Try it out for yourself—here are a few questions you can ask yourself to identify your own strengths:
- What do you enjoy doing?
- What do you do well?
- How can you harness these strengths to help better deal with the stress of managing your diabetes?
“Even if it seems like it’s hard you can actually do it. You can learn how to count carbs, and you can learn how to give your own shots, and you can learn how to do things. Don’t think you can’t do it, because you can do it.” – Cody, age 10, living with T1D
Your medical team, caregivers, family and friends can all be part of promoting resilience as well. Family members can offer support and compassion. Friends and colleagues can inform themselves on how to respond in a hypoglycemic emergency. Partners and other diabetes caregivers can come with you to your doctor’s appointments and provide reassurance that you are not alone. Mental health providers can also work with you to help increase your resilience.
“Having a strong social support network, being able to lean on your partner, other members of your home, as well as having to trust in the technology, being able to utilize as CGM or flash glucometer at night has given me such peace of mind.” – Becca, age 44, parent of child living with T1D
Platforms like Facebook and other social media channels can be a source of support, and help you find peers who have had similar experiences and can relate to what you are going through. Check out the Breakthrough T1D Canada Type One Diabetes Support Group on Facebook, or the Community Activities page for local events. Making connections through an online diabetes community has been associated with lower blood-glucose levels than those who do not—which in itself can help reduce stress.
Technology and resilience
Developing resilience can also involve the resources and tools that you use to manage your condition. Technologies like flash glucose monitors (Flash GMs) continuous glucose monitors (CGMs) and insulin pumps may simplify your diabetes management routine, improve your quality of life and help you feel more in control.
Diabetes management technology may be more beneficial to building resilience for some people than others—if you haven’t considered incorporating this technology into your lifestyle, now may be the time to explore.
“My continuous glucose monitor is a tool that I can’t do without, that gives me a sense of freedom, that allows me to do activities without the fear of severe hypoglycemia.” – Henri, age 32, living with T1D
Seek Out Supportive Communication
Resilience is associated with strong social support. When reaching out to others for support when feeling stressed by the challenges of managing T1D, it is important that the people you look to for support provide encouragement, rather than criticism or judgment.
Here are a few examples of critical versus supportive language. If you find that your friends and loved ones often make comments that resemble the phrases on the left, you may want to try and discuss positive reinforcement by sharing these examples with them.
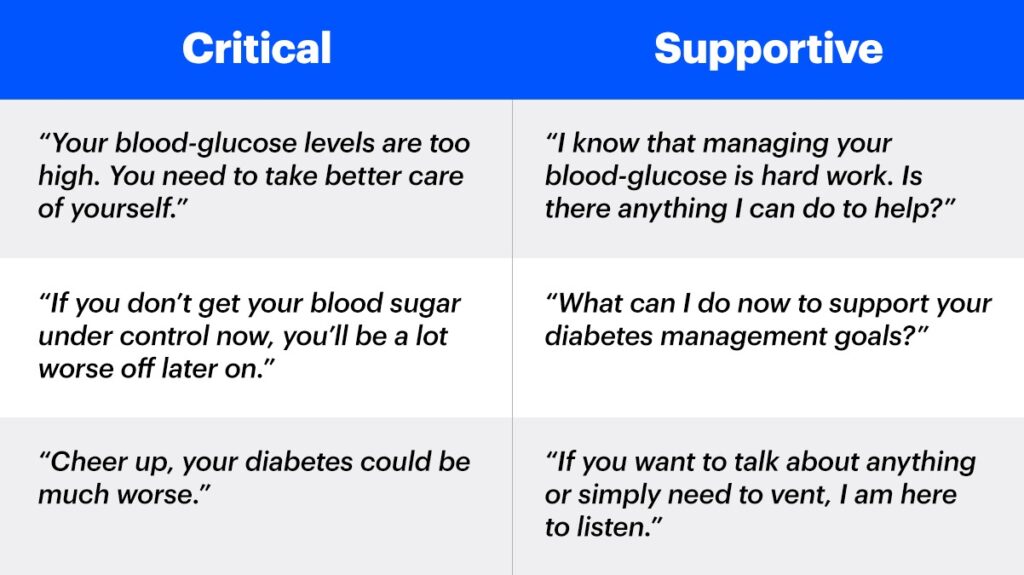
Aside from offering to help out or lend an ear, it can also be effective for others to acknowledge the efforts and successes of people with T1D. Recognition of your progress can provide positive reinforcement and help keep you motivated.
“I think of my family, my friends who have been there every time I’ve had to face difficulties because of my diagnosis, who will be there for the difficulties to come.” – Henri, age 32, living with T1D
What is diabetes distress?
Diabetes can be a difficult and demanding condition. The daily ongoing demands of managing type 1 diabetes (T1D) as well as any diabetes emergencies, development of complications, health issues, or even modifications in your treatment plan like changing insulins or starting a new flash glucose monitor (Flash GM) or continuous glucose monitor (CGM), can add to the emotional burden of diabetes. This can lead to significant diabetes distress.
Diabetes distress is defined as a range of emotional responses to living with and managing diabetes. This can include feeling overwhelmed with the burden of managing diabetes; fear and worries about complications or experiencing a severe low; feeling defeated, discouraged, or burned out when you are not meeting your blood sugar goals despite your best efforts to manage them.
“I felt that if I expressed how truly unhappy I was with my disease that it would be seen as a weakness. So I decided to just keep those feelings inside and not deal with them, which of course just resulted in feeling more isolated and more by myself.” – Sarah, age 33, living with T1D
Experiencing diabetes distress is a normal reaction to living with diabetes. In fact, it’s a common problem that affects one-third to nearly one-half of adults and youth with diabetes.
Diabetes distress doesn’t only affect the person living with diabetes, but family members like parents and partners can experience it as well.
Diabetes distress or depression?
There are no vacations or breaks from T1D and managing it can be frustrating. Studies have shown that the majority of people living with diabetes experience worries, fears and negative feelings, which can lead to diabetes distress.
Diabetes distress differs from major depressive disorder in many ways, but the two conditions often overlap and share some similar symptoms. Because of the similarities, diabetes distress can be misdiagnosed as depression, which can lead to individuals receiving the wrong treatment for it. This misdiagnosis is also due in part to the similarity of common depressive symptoms with symptoms related to high blood sugar levels – like fatigue, weight loss, and issues with sleeping.
Compared with major depressive disorder, diabetes distress is:
- Diagnosed in people with diabetes
- Not considered to be a psychiatric disorder
- Far more common than depression
- Unlikely to respond to medications
- Often directly linked to poor glycemic management and poor self-care (even at low levels of distress)
However, diabetes distress is treatable, highly responsive to clinical attention, and is not an inevitable part of living with T1D.
Dealing with diabetes distress
It is important to learn how to cope with your feelings of distress, worry, and burnout and get help from your healthcare team. Here are some tips:
- Acknowledge your feelings. You won’t feel happy all the time, this is normal! Almost everyone with diabetes has felt frustrated or stressed about the challenges of managing it. But when feelings get overwhelming and last more than a week or two, you might need help.
- Talk with your diabetes care team. Getting help from your diabetes healthcare team (doctor, nurse, diabetes educator, psychologist, or social worker) is important to treating diabetes distress. It’s important to get help early! Your diabetes healthcare team can help by assessing your diabetes distress and developing a management plan to address the challenges you are having. They may also refer you to another healthcare provider. Always remember to advocate for yourself and your care when you need extra support!
- Get support. Talk with your family and friends and tell them how you’ve been feeling. Be honest about your feelings and tell your loved ones how they can help you (most people don’t know what they can do – and maybe you just want someone to listen to you vent).
If you feel uncomfortable talking to family or friends, you may want to join a support group. Sometimes talking to other people with T1D who understand what you are going through can help. A shared experience offers a different type of support than friends and family. People with diabetes who get support do better – managing their diabetes, how they feel and their quality of life. - Set realistic expectations for yourself. Taking one thing at a time, in small doable steps, can lead to big improvements. Set small SMART (Specific, Measurable, Achievable, Relevant, Time-Bound) goals for yourself like “check my blood sugar 4 times today” and then once you are doing that set another small goal like, “walk 10 minutes a day two times a week.” Once you achieve one goal, add another small goal or increase the frequency of your goal. Your diabetes treatment team can help you set these goals.
- Take time to do things you enjoy and reward yourself. Give yourself a reward when you meet your goals. This should be something you enjoy — watching a movie, hiking, playing a game, or spending time with friends (it doesn’t need to cost money). It’s important each day to spend time doing something you enjoy and having some “me” time to reward yourself for meeting your goals.
When to ask for support
If your diabetes management is off track, ask for support. You may need a treatment change, or outside stressors like work or relationship challenges might be affecting you more than you realize.
It may be useful to take a step back to determine what the problems are and get support. Talking to other people who understand is very important. Breakthrough T1D has resources to help connect you to others in the T1D community or a mental health provider.
Type 1 diabetes and depression
People of all ages experience depression. According to the World Health Organization, over 280 million people globally experience depression, but it often goes undiagnosed and untreated because of the stigma around mental health issues.
Depression is estimated to affect one in four people with diabetes (type 1 and type 2). Adolescents with type 1 diabetes (T1D) have five times the rate of depression than adolescents without the condition.
Having T1D doesn’t mean you will develop depression, but being aware of the symptoms is important so you can recognize them early and get treatment.
Symptoms of depression in adults include:
- Feelings of sadness or hopelessness
- Loss of interest or pleasure in activities you used to enjoy
- Changes in sleep – either too much or not enough
- Changes in appetite – either eating too much or not enough (and sometimes changes in weight)
- Tiredness and lack of energy, so even doing small thing take extra effort
- Slowed thinking, speaking or body movements
- Trouble concentrating, making decisions, or remembering things
- Feelings of worthlessness or guilt, fixating on past failures or self-blame
- Frequent or recurrent thoughts of death or suicide attempts
“My physical symptoms of diabetes were only the tip of the iceberg. Beneath the surface was anxiety, depression, shame, guilt, fear, and the stigma that came from having diabetes.” – Christine, age 34, living with T1D
In children and adolescents, symptoms of depression can be similar, but there may be some differences. In children, symptoms may also include:
- Clinginess
- Irritability
- Body aches and pains
- Refusing to go to school
- Poor performance in school
In older children and teenagers, symptoms may also include:
- Irritability and anger
- Poor performance or poor attendance at school
- Feeling misunderstood
- Being extremely sensitive
- Avoiding social activities
- Possible use of recreational drugs or alcohol
Across all ages the symptoms of depression interrupt or greatly affect work or school, social relationships, or other important areas of their lives.
Treatment
The good news is that depression can be treated and symptoms diminished, especially when depression is diagnosed and treated early.
It is recommended that individuals with diabetes should be regularly screened by their healthcare providers for depression, so treatment or a referral to a mental health provider can be made.
If your healthcare provider doesn’t ask about how you are feeling emotionally – it is very important that you speak up and tell them. Getting treatment for depression early is key and can help to improve your long-term physical and mental health outcomes.
Treatment for depression in children and adults can include cognitive-behavioral therapy (CBT), interpersonal therapy or other evidenced based therapy and/or medication(s). Finding a mental healthcare provider who is knowledgeable about diabetes can also help. In September 2023, Breakthrough T1D, , in collaboration with Diabetes Canada, launched the Mental Health + Diabetes Directory, to easily help you connect with a mental health provider that is knowledgeable about diabetes.
Type 1 diabetes and sleep disruptions
Sleep in people with type 1 diabetes (T1D) and their caregivers can be a challenge. The quality and quantity of sleep (or lack thereof) has been talked about by people living with T1D for years; however, with the new devices and alarms now on the market, it has gained the attention of researchers and clinicians.
People with T1D have interrupted sleep on a regular basis – from needing to urinate during the night because of high blood sugars and then correcting; waking to treat a low blood sugar and then having difficulty falling back to sleep; setting alarm clocks to check blood sugars; waking to high or low CGM alarms etc.; or even worries about T1D can keep you up at night.
“Fear seems to be a synonymous term with diabetes. Worrying that your child is going to fall asleep and go incredibly low, or incredibly high or not wake up, is par for the course and that’s the scary part of our reality.” – Becca, age 44, parent of a child living with T1D
Because parents of children with T1D manage their child’s blood sugar (and worry a lot more about diabetes than their children), they experience this same disrupted sleep.
Recent research has documented sleep loss because of diabetes disruptions, both anticipated and unanticipated of up to 10 hours a week.
Sleep is important to good cardiovascular and metabolic health. Children, adolescents, and adults who reported less sleep also have higher blood sugar levels. Also, people with T1D who have sleep disruptions or lack of sleep are less insulin sensitive and need more insulin the following day after not sleeping well.
Tips for better sleep
There is no magic bullet to help people with T1D or their caregivers get better sleep. But you can use some tips to get a better night (and more) sleep.
- You should first make sure that you (or your loved one with T1D) do not have any medical issues contributing to your sleep issues. New research has shown that obstructive sleep apnea (OSA) is more common among people with T1D than those without diabetes. People with OSA stop breathing repeatedly and then start again throughout the night. Make sure to talk to your doctor to rule out a treatable sleep disorder.
- Talk to your healthcare provider about setting CGM alarms to a different setting at night for high and low blood sugars to reduce alarms.
- If your diabetes worries are preventing you from sleeping, talk to your doctor or your child’s healthcare provider. They can give you tips for managing blood sugars throughout the night and can assess if your fear of hypoglycemia could be a barrier to good rest.
- Get into a routine – try to go to bed at the same time and get up at the same time every day (including weekends).
- Get regular physical activity – being active during the day can help you fall asleep as well as improve your emotional well-being.
- Avoid caffeine, alcohol, or eating a lot right before you go to bed.
- Create a relaxing sleeping environment – make sure your bedroom is quiet, the blinds are shut (keeping the light out), and at a comfortable temperature.
- Keep electronics out of your bedroom, including computers and TVs, and minimize how much you are on your phone before bed.
Getting a good night’s rest is important for everyone’s health and well-being. Although T1D will interrupt your sleep at times, getting regular sleep is important for your long term health.
“Knowing that I can check my child’s blood sugar without having to wake him or poke him and just know how his night will transpire, allows us all to sleep better.”— Becca, age 44, parent of a child living with T1D
Type 1 diabetes and disordered eating
Eating disorders are relatively common in people with type 1 diabetes (T1D). In fact, nearly 1 in 5 children with T1D, and 1 in 4 females, show signs of disturbed eating behaviour. Mental health issues, family circumstances, and environmental factors can all play a role in developing disordered eating habits.
After T1D is diagnosed and insulin therapy has started, people experience weight gain, restoring the weight they lost before diagnosis, which may or may not contribute to worries about weight gain and body image.
People with diabetes who have eating disorders also have high rates of fear of hypoglycemia, diabetes distress, and other psychological diagnoses such as depression. So, getting treatment for eating disorders is important for short and long term health and well-being.
Insulin Omission to Lose Weight (“Diabulima”)
People with diabetes and eating disorders—men and women alike—often face the same feelings about weight and body image as people without diabetes. But there is an additional way that people with T1D may try to lose weight – if they restrict or omit their insulin. For people with T1D, insulin omission to lose weight is the most commonly reported disordered eating behavior, often referred to as “diabulimia”.
When people try to lose weight by manipulating their insulin, they purposefully take less insulin than is required to induce hyperglycemia or diabetic ketoacidosis (DKA). DKA can be very dangerous and can lead to coma or death. If you are experiencing these symptoms, it is important to call your health care provider and/or go to your local emergency room right away.
“At 12 years of age, I felt as though if I could change my body, I could change the way diabetes made me feel. I began dieting and developing disordered eating habits. Later on in my teenage years, this self-perception evolved into diabulimia.” – Christine, age 34, living with T1D
Symptoms of DKA include:
- Thirst
- Frequent urination
- Ketones, when you check them by using a urine stick or fingerstick
- Nausea and vomiting
- Shortness of breath
- Fruity-scented breath
- Feeling tired or fatigue
Unfortunately, short-term weight loss can be motivating to people, despite the short and longer-term risks of keeping blood sugars high which can lead to serious complications. Other signs of insulin omission can include:
- High HbA1C (typically over 9.0%)
- Episodes of diabetic ketoacidosis (DKA)
- Concerns about weight and body shape regardless of current body size
- Exercising a lot
- Changes in eating patterns (often restricting food and then binge eating)
- Skipping monthly menstrual periods (amenorrhea)
- Behavioural changes (e.g. secretive behaviour)
Not all disordered eating has to do with restricting or omitting insulin. People with T1D experience other eating disorders just like the people without diabetes.
Other eating disorders
Anorexia nervosa
There are both emotional and behavioural aspects to anorexia. A person with anorexia has an unrealistic perception of their body or a strong fear of being fat, or both. To lose weight they restrict their food intake and/or binge eat and then make themselves vomit or take laxatives. They also tend to exercise excessively.
Bulimia nervosa
There are also both emotional and behavioural aspects of bulimia. A person’s self-worth is based on their weight and shape. They have reoccurring episodes of binge eating and a lack of control over what and how much they eat during the episode. After binging a person makes themselves vomit or takes laxatives to compensate for what they ate to prevent weight gain.
“I myself have bulimia…Not only is it a disease but it is an addiction. I’m addicted to negative thoughts towards my food and gaining weight. It then overwhelms me and increases my anxiety to even take insulin.” – Jessica, age 36, living with T1D
Binge eating disorder
People who have binge eating disorder have reoccurring episodes of binge eating and a lack of control over what and how much they eat during the episode. They feel embarrassed by how much they are eating and feel disgusted or very guilty afterwards, but they do not make themselves vomit or take laxatives to compensate for what they ate.
Treatment
If your healthcare provider doesn’t ask about your feelings regarding your weight and eating, it is important that you speak up and tell them! Getting treatment early is key for any disordered eating is important and can help to improve your long term medical and psychological outcomes.
Treatment for disordered eating is a multidisciplinary approach and includes endocrinologists, nurses, dietitians, and mental health providers. In both children and adults this can include cognitive-behavioral therapy, family therapy or other evidenced based therapy, as well as diabetes education, and nutritional counselling. Finding a mental health provider that is knowledgeable about diabetes can help. The Mental Health + Diabetes Directory is a tool to find a mental health provider near you. If you are looking for support on eating disorders, you can access the National Eating Disorder Information Centre’s directory.
If you are struggling with disordered eating or restricting insulin to manage your weight, talk to your diabetes care team.

T1D resources and support
Explore our list of FREE mental health resources, make a personal connection with someone experienced with type 1 diabetes (T1D), or check out our Mental Health + Diabetes Training Program to learn more.
“Breakthrough T1D (then JDRF) helped connect us with a mentor. That was a huge resource to me, to meet someone else that was going through the same thing as I was, was so helpful emotionally but she also opened my eyes to all the resources that were out there” – Jen, age 48, parent of child living with T1D
Get support
Talking with your friends and family is key. They want to help you, so asking for what you need (rather than having them guess or do something unintentionally unhelpful) is important.
Depending on your relationships with your family and friends, it may be difficult to talk to them. You may find that talking to other people with T1D can be more helpful. Many people have found joining a local diabetes support group at their diabetes education centre, local hospital or joining one online to be a valuable form of community. There are many types of support groups, and it’s best to find the type that meets your personality and needs. You might want to consider checking if there are support groups at your hospital or doctor’s office or participating in Breakthrough T1D’s Connection Series to get support.
“You can just talk about what’s relevant to you right now with type 1 diabetes. It can be asking questions, talking about a hard day, and you can relate to other families which is kind of one of the best ways to talk about all the anxiety and stress that goes along with type 1 diabetes. – Jen, age 48, parent of child living with T1D on the Connection Series
When to seek help from a mental health provider
It’s important to seek out the help you need in order to cope with the mental challenges that come with T1D—but how do you know that a mental health provider is right for you?
You may need some extra support if you’re:
- Lacking the motivation to check your blood sugar or take your insulin.
- Feeling like your mental health is getting in the way of diabetes management.
- Having trouble navigating your relationships with family and friends.
- Avoiding your loved ones because you are not up to being around other people.
- Forgetting about things that are important to you — not wanting to participate in hobbies or activities that you normally wouldn’t want to miss out on.
If you’re feeling this way, you’re not alone. If you’re unsure whether this is the right option for you, talk with your healthcare team. Finding a mental health provider might seem like a big step, but it can make an even bigger difference.
Remember: The feelings and challenges you are experiencing—depression, anxiety and everything in between—are struggles faced by many people, whether they have T1D or not. It is very possible that a general therapist can provide you with the help you need.
There is a chance that your endocrinologist does not have a recommendation for a mental health provider. Insurance, cost, availability and geography may also present challenges and limit your options. However, there may be publicly available services in your area available through a doctor’s referral, or virtual care options which can allow you to select the provider that is right for you.
How to find a mental health provider
Finding the right medical team to help you manage your physical health when you have T1D is very important–but the importance of your mental health should not be overlooked. Therapy might be a helpful step in developing coping skills to overcome these challenges and build resilience.
Whether you’ve been living with T1D all your life, or you were just diagnosed, you know that diabetes management impacts your day-to-day life in countless ways. Transitioning into this routine, or even maintaining it after many years, can take a toll—and there’s no shame in getting some help. Talk to your healthcare team about a referral to a mental health provider.
In September 2023, the Mental Health + Diabetes Directory launched, a connection tool to easily find a mental health provider that has received specialized training on diabetes.
“There are so many different facets to managing type 1 diabetes. It’s similar to putting together a puzzle. Except this puzzle has infinite pieces, no outline, no corners, and sometimes the pieces fit and sometimes they don’t” – Alison, age 51, parent of teenager living with T1D
Resources
- Find a mental health provider
- Explore free mental health resources
- Connect with the T1D community
- Link up with peer support
- Join our Facebook T1D support group
- Find local community activities
- Get tips on exercise with T1D
- Are you a healthcare provider?
- Take the Mental Health + Diabetes Training Program
- Newly diagnosed
- Mental Health Research