A significant part of JDRF Canada’s research strategy is funding the most promising cure-based research for type 1 diabetes (T1D).
T1D is an autoimmune disease where the body destroys the cells in the pancreas responsible for making insulin. People with T1D must administer external sources of insulin, either through multiple daily injections, pump or pen in order to survive. Many cure-based research studies involve replacing these cells through transplantation, in the hopes that they will start producing insulin again.
Transplantation of donor cells could be a possible cure for type 1 diabetes
Transplantation of donor pancreatic islet tissue is a promising therapy; however, transplant therapy is limited due to shortage of transplantable islets (from deceased donors), limited durability of transplanted cells (cells that stop working or growing after transplantation), and the need for long-term immunosuppression therapy to prevent immune-based rejection of the transplanted cells, similar to organ transplants. Identifying alternative and more universal sources of transplantable beta cells is necessary to make this potential therapy available to larger numbers of people living T1D, and the Nagy lab is dedicated to achieving this.
How does it work?
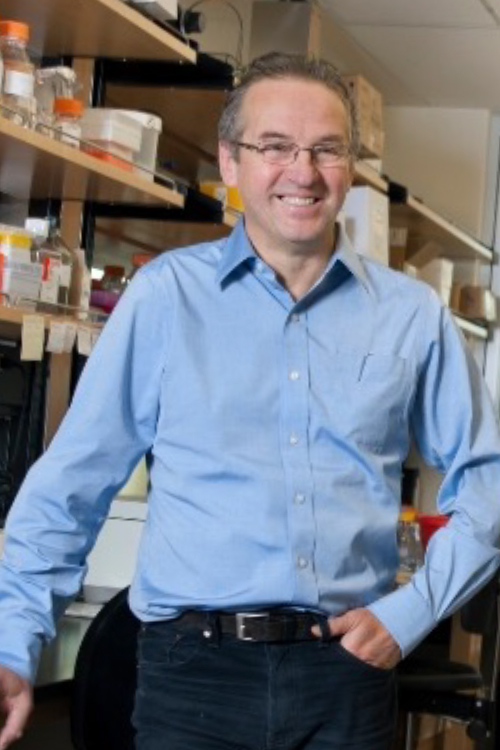
In a brand-new JDRF funded project, Dr. Andras Nagy, senior investigator at the Lunenfeld–Tanenbaum Research Institute in Toronto, Canada, is testing the functionality of insulin-producing cells created from human stem cells. In collaboration with Dr. Timothy Kieffer (University of British Columbia), Dr. Nagy’s team will cultivate insulin-producing islet cells from an unlimited supply of human stem cells for a potentially unlimited cell therapy.
These cells will incorporate two gene-editing technologies previously developed and patented by the Nagy lab: (1)Dr. Nagy’s FailSafeTM technology is a gene-editing solution that employs an inducible kill-switch to rapidly eliminate dividing, potentially tumour-forming, cells, thereby eliminating the risk of tumours following transplantation of a stem cell-derived cell product. (2) Dr. Nagy and his colleagues have developed an “immunocloaking” strategy for the transplanted cells by modifying specific genes that allow these cells to remain hidden from an immune system attack.
These technologies will offer solutions to the safety concerns of cell therapy and the autoimmune challenge found in T1D, which could allow for stem cell transplants without the need for immunosuppression.
This is an exciting project that harnesses the most cutting-edge methods to develop a safe and effective cell therapy solution that may lead to a cure for T1D.
JDRF Canada will provide updates on this research as it becomes available, and when it moves to the clinical trials stage.