May is Mental Health Awareness month, a national movement to raise awareness of the importance of mental health and the structural gaps that exist in accessing treatment and support.
Mental health is central to living well with type 1 diabetes (T1D). This is why, in 2021, Breakthrough T1D Canada launched its Mental Health Strategy, with the goal of better supporting mental health in people with T1D, while we continue to support research towards cures.
T1D affects a person’s emotional, social, and mental wellbeing throughout their lifetime, known collectively as psychosocial health. Psychosocial challenges can negatively impact diabetes outcomes like glycemia. Many people with T1D experience “diabetes distress” – a term describing the powerlessness, stress, guilt, relentless worry and denial that accompanies living with diabetes and the burden of self-care. In addition, people with T1D are at higher risk of mental health disorders including depression, anxiety and disordered eating. These challenges are common in people with T1D and can be treated – but they are often underappreciated or undertreated because of gaps in care and support.
To better address these areas of need, Breakthrough T1D outlined a three-pronged approach to its Mental Health Strategy: 1) knowledge generation through new research, 2) a new training program for mental health providers, and 3) development of new community supports. Since 2021 when we laid the foundations of this strategy, we have driven substantial progress in all three key areas, thanks to the generous support of donors, as well as partnerships with academia, other diabetes organizations, and community collaborators.
We are pleased to share the updates to this program that have taken place in the past year.
Research Update
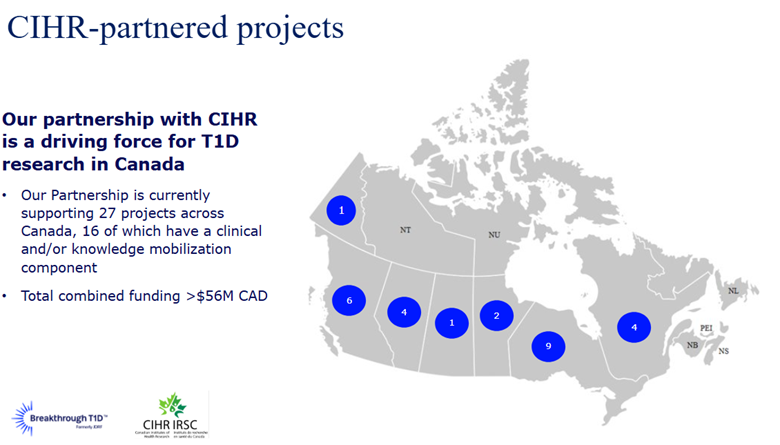
Since the launch of our mental health strategy in 2021, we have invested $5 million in new research focused on T1D and psychosocial health, together with partners including Brain Canada, the Canadian Institutes of Health Research (CIHR), and Michael Smith-Health Research BC.
This includes funds from Breakthrough T1D Canada, Brain Canada, CIHR, and MSFHR
9 awards total:
- 3 with Brain Canada
- 4 with CIHR
- 1 impact award (BT1D only)
- 1 partnered award to Dr. Tricia Tang (Michael Smith-Health Research BC)
All the new research funded is still in progress. In line with our global research strategy in this area to build programs that are designed to scale up and ultimately help larger numbers of people, many of the projects we are supporting involve development and testing of digital interventions. For example, Dr. Tricia Tang and her team at the University of British Columbia (UBC) carried out a clinical study of their virtual peer support platform called REACHOUT. This platform uses a mobile app to deliver peer-led mental health support by trained mentors to adults living with T1D in rural and remote regions of BC. The trial assessed the effects of virtual peer support on outcomes including diabetes distress, quality of life, and HbA1c. Future work will focus on iterative improvement of the REACHOUT platform and scaling up the reach of trained mentors so that more people with T1D can be supported.
Other studies that are leveraging digital technologies to engage people with T1D across Canada include that of Dr. Deborah Da Costa at McGill University, whose study is testing how best to support the mental health and wellness of women with diabetes during pregnancy, and that of Dr. Holly Witteman from the University of Laval, who is developing a network of virtual peer support for people with T1D with specific needs and interests.
Other Breakthrough T1D-supported research is focused on improving outcomes around the transition from pediatric to adult care, a life stage when many youth stop seeing their endocrinologist, which can lead to challenges such as rising HbA1c, isolation, stigma, and eating disorders. Dr. Sonia Butalia at the University of Calgary is carrying out a clinical trial of a system designed to improve this transition, which saw improved blood glucose levels among those involved in the program’s initial pilot in Calgary. In the latest trial funded by Breakthrough T1D and CIHR, the program, which consists of a transition coordinator and carefully designed communications, is being scaled to other Alberta Health Services (AHS) sites in Calgary, Edmonton, Lethbridge, Medicine Hat, and Red Deer.
These clinics and community partners are very keen on the team’s transition work, and AHS has approved the budget for this project to be sustained past the life of the grant. Translation of this work would mean that this demographic of people living with T1D will no longer fall through the cracks during the transition from pediatric to adult care.
“My son Luke has lived with T1D since he was 5 years old, and now he is a teenager. It has been a big challenge for him and our whole family, and though Luke is well-supported, in large part due to his involvement with Breakthrough T1D, adolescence and early adulthood bring a whole new set of challenges. I am so glad Dr. Butalia and her team are implementing a model of transition-age care that hopefully will be able to help Luke in a couple of years. It’s great to see this vital research being scaled across Alberta and ideally expanded across the country.” -Ryan MacDonald, Calgary, Breakthrough T1D Campaign to Accelerate Co-Chair.
Mental Health + Diabetes Training Program
Many people with T1D face mental health challenges that require the support of a registered mental health provider – ideally one who understands the unique mental health challenges posed by diabetes. To help inform Canadian mental health providers about diabetes, Breakthrough T1D launched the Mental Health + Diabetes Training Program in early 2023, in collaboration with Diabetes Canada.
This fully bilingual course is offered virtually as two streams: one for registered Canadian mental health providers (which includes a live facilitated session focused on clinical competencies), and one for other healthcare providers and the public that consists only of self-guided modules. The course is delivered at no cost, provides 10 Continuing Education credits for selected providers, and has been approved by the Canadian Psychological Association as well as other associations.
As of May 2025, over 500 mental health providers have completed the program thus far, and over 1000 others (other types of healthcare providers, or members of the T1D community) have enrolled in the training. Early outcomes of the training program’s impact have recently been published as a peer-reviewed paper in the Canadian Journal of Diabetes. An additional evaluation study is in progress that will assess the impact of the program on trainees’ clinical practice.
Development of Community Supports
The T1D community is diverse and includes many subgroups with varying psychosocial needs and challenges. Towards meeting this need, in the first three years of our strategy, we strove to develop community supports through several different activities, with the help of our dedicated Mental Health Advisory Council—a group of >100 volunteers with diverse lived experience of T1D. In the past year, we continued to expand our sources of community support in a number of ways.
First, we delivered several virtual events to engage and educate our community:
- Over 500 individuals attended our Breakthrough T1D Education Series – T1D and Mental Health sessions in May 2024 (in English and French).
- Nearly 200 healthcare providers attended sessions on T1D and eating disorders (in English and French) hosted in collaboration with the National Eating Disorder Information Centre (NEDIC). These webinars helped increase dialogue and learning opportunities for healthcare providers and others.
- Over 500 people attended our Breakthrough T1D Education Series – Disordered Eating and T1D. These bilingual events featured speakers from NEDIC, ANEB (Anorexie et boulimie Québec), and people with lived experience and explored the realities and challenges of managing T1D-related eating disorders. By fostering dialogue on this underappreciated topic, we hope to see eating disorders recognized and treated more effectively, leading to better care and outcomes for those impacted.
Second, we expanded our Directory of mental health providers who have been trained in diabetes through our new training program, as a resource for people with diabetes or healthcare teams to connect with a mental health provider with knowledge of their disease. As of May 2025, we list >180 providers from across Canada and anticipate that listings will grow over time as more providers are trained.
Third, we monitored progress and facilitated the success of projects funded through our inaugural Mental Health and T1D Community Grants program, a mechanism to catalyze the efforts of other organizations to develop new community-facing programs designed to support and improve mental health and wellness in the T1D community. The first grants awarded through this program are progressing well through their 18-month term, and updates will be provided upon their conclusion in late 2025.
Finally, we are pleased to share a new video series to share stories from our community: Beyond the Numbers: Real stories of navigating mental health with T1D. We will be sharing these videos throughout Mental Health Awareness Month and beyond, to help normalize the psychosocial problems, solutions, and wins that are part of daily life with T1D. Featuring 20 videos, this series addresses themes of Relationships and Social Support, Life Transitions, and Coping and Resilience.
Thank you to our community
Breakthrough T1D Canada remains enormously grateful for the support of our Mental Health Advisory Council, lead volunteers and philanthropic partners, including funding partners Brain Canada and Diabetes Canada, without whom our progress in this area would not be possible.
For more information on mental health supports, please visit the Directory at directory.breakthroughT1D.ca or our mental health resources page.
T1D community resources & events
Web resources and blogs