JDRF congratulates the McGill University Health Centre (MUHC) on its recent mandate to provide islet transplantation for persons with T1D in Quebec. This designation by Quebec’s Ministry of Health and Social Services recognizes the clinical and research teams at MUHC for their leadership and dedication in the field of islet transplantation. As one of only a dozen treatment centres in North America able to perform islet transplantation, this designation also means that the MUHC will be able to improve access to their services and treat more individuals.
JDRF’s Global Research Strategy focuses on funding research that has a high likelihood of accelerating the development and availability of type 1 diabetes (T1D) treatments, as well as improving the lives of people who live with T1D. Cell therapy treatments in particular hold a lot of potential, as they may become a meaningful treatment option leading towards insulin independence. JDRF is committed to funding research to make cell therapy safer and more accessible for people with T1D. JDRF is proud to have continually supported the development of cell therapies for decades. Over 20 years ago, JDRF funded both the team lead and the pre-clinical trials that lead to the Edmonton Protocol, which revolutionized the procedure for islet transplantation. Today, JDRF supports many projects that research cell therapies, including continuing research into refining islet transplantation.
Currently, replacing damaged islets is the only treatment that is clinically proven to be able to achieve insulin independence in people with T1D. Even in cases when complete insulin independence is not achieved, islet transplants can be life changing for people with T1D who experience severe hypoglycemia and hypoglycemia unawareness, for example. The treatment is minimally invasive and much lower risk than pancreas transplantation.
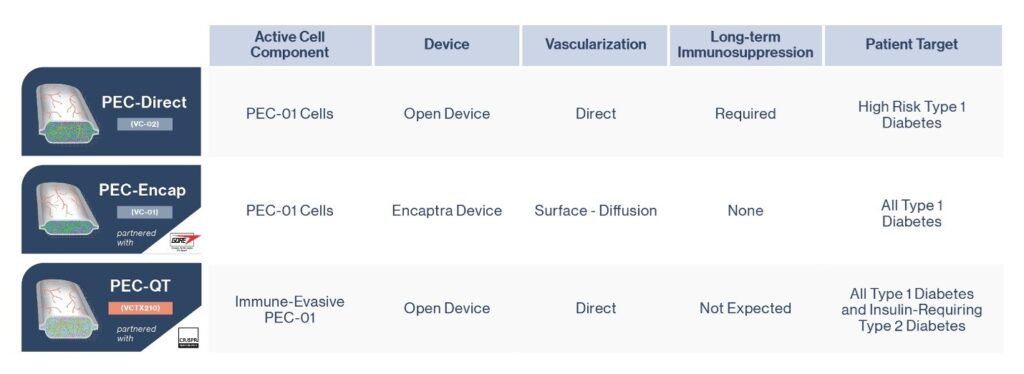
However, barriers to making islet replacement therapy more efficient and accessible remain. The transplant of donor islets requires recipients to take lifelong immunosuppressants, which can have risks and side effects. There is also a limited supply of donor islets, which limits the amount of people who can receive this treatment. JDRF researcher Dr. Timothy Kieffer, PhD, is one of several JDRF-funded researchers who is currently examining ways to overcome these limitations through gene editing and stem cell technologies. Other factors, such as poor blood supply to the transplanted islets, can also affect the success of islet transplants. JDRF-funded work in Dr. Michael Sefton’s bioengineering lab is exploring solutions to this issue. Recipients may also need additional infusions of islets in the years after the initial treatment to maintain insulin independence, as transplanted islets may not be a lasting solution. And so, although ongoing research and trials are promising, many hurdles remain before islet replacement therapy is widely accessible to people with T1D.
Research at the MUHC facility is also exploring ways to overcome these challenges in islet transplantation. The MUHC team is led by Dr. Steven Paraskevas, a transplant surgeon, researcher, and Professor of Surgery at McGill. In addition to his role as Director of the Human Islet Transplantation Laboratory, he is Director of Pancreas and Islet Transplantation at the Royal Victoria Hospital and former President of the Canadian Society of Transplantation. His research focuses on beta cell injury and survival, as well as the way beta cell injury stimulates the immune system. Understanding beta cell injury is crucial in figuring out how to ensure transplanted islets survive longer and better, with less need for additional transfusions. Such research is essential for advancing knowledge to ensure that opportunities for islet replacement therapy increase in the future, as clinical trials are still at relatively early stages.
The MUHC is also a site for collaboration, with industry partners as well as with other teams of scientists. The MUHC is currently the site of a clinical trial in conjunction with Vertex Pharmaceuticals. Vertex is conducting a clinical trial of VX-880, a new stem-cell derived therapy for T1D, at several sites in North America (of which the MUHC was the first Canadian site, and Toronto is now recruiting participants as well). The VX-880 product uses islets derived from stem cell cultures rather than from donated pancreases. By using stem-cell derived islets, VX-880 could make islet transplantation and insulin independence available to a greater number of people, if Vertex’s trial program goes on to show safety and efficacy. The clinical trial is still ongoing, but early results out of the US trial sites are promising. The patients who have so far received VX-880 have shown improved blood glucose time-in-range with fewer insulin injections.
The MUHC further supports research by housing the McGill University Health Centre Human Islet Transplant Laboratory, which purifies islet cells from donated pancreases. These cells can then be transplanted into patients as well as being used in research to further our understanding of islet biology and the pathogenesis of T1D. The MUHC’s designation as a provincial centre for islet transplantation will help to ensure that cell therapy treatments will continue to develop.
The Vertex trial is currently recruiting participants with T1D for their trial in Montreal and in Toronto. To see if you qualify, click here.