Miguel Alvarez, who has been living with type 1 diabetes for over 55 years, aims to complete two bike rides of over 100 miles each.
To mark his 55th ‘Diaversary’ – the date when someone was diagnosed with type 1 diabetes (T1D), Vancouver, BC resident Miguel Alvarez will be attempting two 100-mile bike rides: the first in Coeur d’Alene, Idaho in September, and the second in Death Valley, California the following month in October. Training for these rides requires dedication, discipline and perseverance, much like daily life with T1D. Miguel will need to put in many hours on the bike but believes if he can help further progress to find a cure for T1D, it will be worth the effort. It’s why he rides.
JDRF was recently able to talk with Miguel, learn more about his five plus decades living with T1D, what drives him to set these ambitious bike ride challenges, and what he hopes to achieve with his fundraiser.
***
I’m originally from Ontario. I’ve worn a few hats in my life. I used to be a professional musician as a drummer and played in the Toronto area in a number of bands and pretty much every music venue throughout Southwestern Ontario. I’ve also worked as a motorsports photographer, and I presently work in technology, after moving to Vancouver.
I was three years old, in 1969, when I was diagnosed with type 1 diabetes. This is now my 55th year living with T1D. One of my earliest childhood memories is being in the hospital, after being diagnosed. It was a traumatic experience. Having visitors was a difficult thing back then, family visits were limited and nobody under the age of 12 was allowed to visit, so my sister couldn’t come to see me. I remember being continually poked with needles, having my blood drawn, things like that. Suffice it to say, these are not nice memories, especially being so formative and some of my first.
And I remember growing up trying to be ‘normal’, but T1D was always present, getting in the way. Much as I tried not to let it affect me. Back then, there was very little in terms of management. We only had one type of insulin. Diet was critical because that was the way to control it. But it was very restrictive. I remember going trick or treating at Halloween and not being allowed to eat any of the candy (it went to my sister) or going to friends’ birthday parties and not being allowed to have any birthday cake. These might not seem like big things, but they were just something else that singled me out as different.
One thing I do feel very fortunate about it is that I was always able as a child to know when I was having a low (hypoglycemia), and I really believe this is one of the reasons I was able to survive 55 years with this condition. I always knew and could communicate to my parents to let them know I wasn’t feeling well, or that I was feeling ‘off’. That I knew I was going low. I’m very lucky that I have always had symptoms of low blood sugar. Many people cannot and that is serious. With the lack of available tools to manage T1D, this was a huge advantage, if you can say that about having this chronic condition.
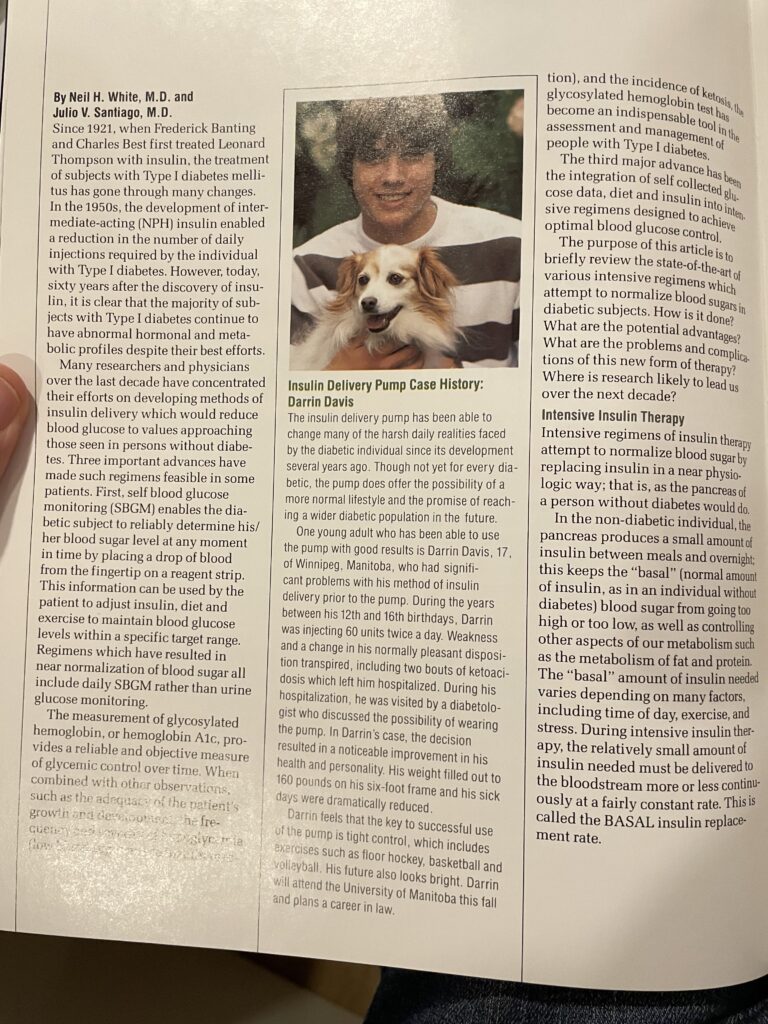
Over time, it is human nature, you learn to live with it (having T1D). I always try to express to people that I’ve basically lived through almost all the advancements of diabetes management, to date. There was no home glucose testing, no different types or better types of insulins, devices like insulin pumps, advanced glucose monitors like CGMs. All the progress in T1D management has directly impacted my life for the better. So, in some way, I feel that I’m a reflection of the best that has come forward in diabetes management, and I can say with certainty that they have not only improved my life but prolonged my life as well.
I’ve always been very open talking to people about diabetes, what it’s like and educating people along the way. The reality is, when I’m asking for money for my fundraiser – I explain that through the research that’s being done, I am a beneficiary of it. It’s not abstract, it’s very concrete. I am one of the few that can say that your donations over the years have benefited me personally.
I’ve found that for people without any personal knowledge of T1D, there is often a misconception that you take insulin and you’re fine. They don’t understand the daily, even hourly management it takes. It’s far more than many people would be able to manage. But it’s something we have to do, every single day. This isn’t about sympathy, it’s just the reflection and reality of living with a chronic disease that affects your everyday life.
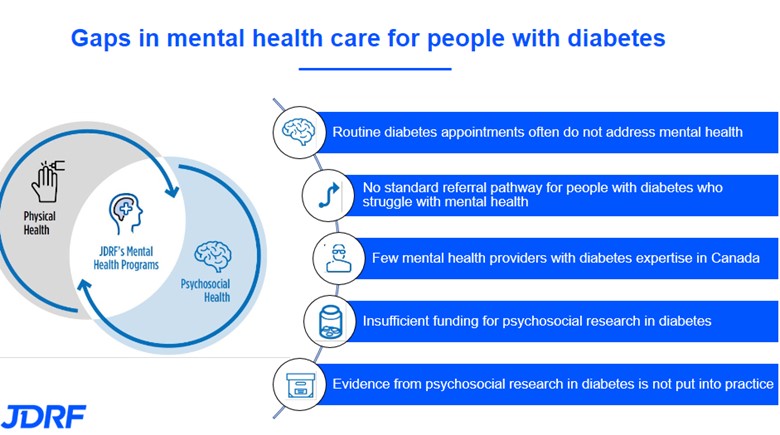
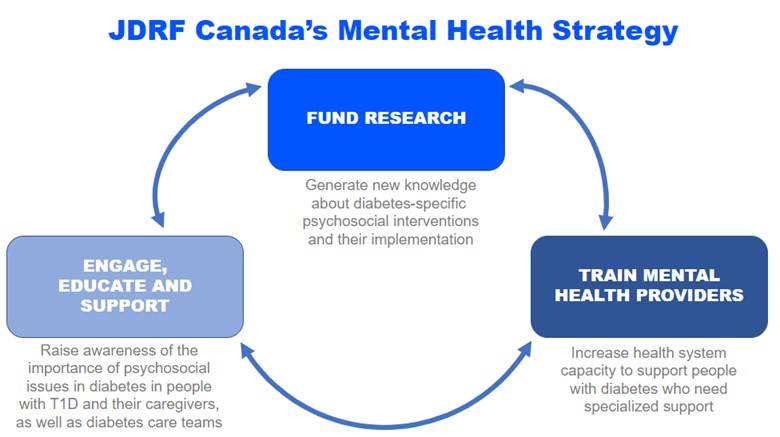
And the mental burden, people don’t always have an appreciation for it. That’s the other aspect. It doesn’t affect just me; it affects everyone around me. My family, my wife, when I’m on a bike ride, I need to be extra vigilant, far more than the average person. It’s not just dealing with one thing; this condition is multi-faceted. And those facets change every day. As much as you try and be consistent, and apply what you think works, there is no explanation when things change or don’t work. No two days are the same. You are always behind the ball. Some days are good, some days are bad. But it’s so hard to juggle all the variables, because you don’t really have control over that. And then there is the tendency to beat yourself up when your control (blood glucose levels) isn’t as good as you want it to be. Then you feel bad. We can be very hard on ourselves too.
Every single day, I think about the potential T1D-related complications, from my eyes to my kidneys to my feet, I’m always thinking about it. And that weighs on me. It’s one thing to live with a chronic condition. But knowing that there are long-term complications that can happen, it’s hard to live with. I’m very concerned about my eyesight. I’m an artistic person. I use my eyes for my work and my creativity. But there is no choice. We do what we must do. And it’s another reason why I am so driven to fundraise to help support critical T1D research.



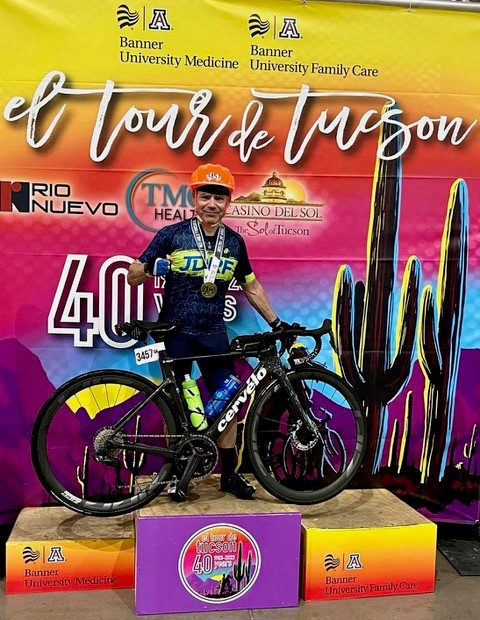

I’ve been doing these bike rides since 2017, in fact, I hadn’t really connected with JDRF until 2016. And when I did, it was the first time in my life that I met people who understood and knew what I was dealing with. It was a huge deal for me. I had never known anyone else with T1D. I grew up alone with this. I didn’t want to just go and ride my bike for the sake of riding, I wanted to do something with it, use it as a tool. I could make a difference, do the thing I love to do, being healthy and riding my bike, and I could raise money for such an important cause and connect with a community, everyone single-mindedly working towards the same goal. I’ve met so many other people now who know what this (life with T1D) is about. I started making friends in the T1D community in the US, and now I go pretty much every year. Working towards these events and raising money – my donors, I keep going back to them, and they keep supporting me. They appreciate that I am doing something so tangible towards T1D research. I do a lot of training to be able to ride 100 miles, and I’m doing it twice in 2024. Which is physically exhausting, but it’s so empowering and so uplifting. It’s quite amazing.
To anyone thinking of becoming involved with JDRF, please know that it makes a difference. And when I say that I use my personal experience knowing what that difference is, and how profound. Everyone’s time and efforts, whether volunteering or fundraising, does have an enormous impact. This is an investment, the results might not be immediate, but we are investing in future generations and in humanity.
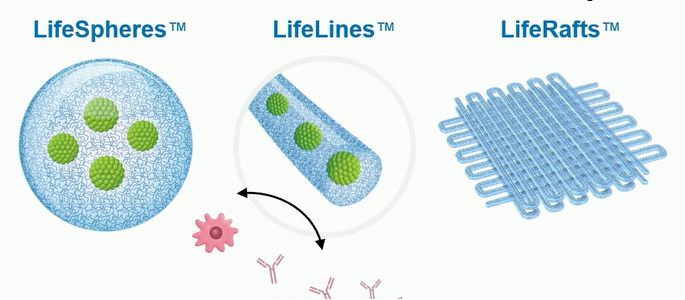
So, towards that end, I’m also in the early stages of participating in a clinical trial, potentially early next year (2025). It seems like I’m a strong candidate. This particular study will implant beta cells (the cells responsible for producing insulin). Essentially, it’s a package of beta cells that are implanted through a surgical procedure. If it works, I wouldn’t need to inject insulin. It’s still early days, but they are interested in me participating. It won’t be easy as I have to be prepared for multiple surgeries. But I know I will get excellent medical attention through the process. I see it as putting my money where my mouth is. I am going to participate directly in finding a cure.
What would a cure mean to me? On the one hand, living with this all my life, it’s become part of my identity. So, if I am no longer diabetic, who am I? It would be a huge mental shift. But not having to manage T1D anymore, would be a whole new life. I would be confident that the future would mean living a less complicated life. My father always used to tell me that they would find a cure in my lifetime, and I want to prove him right. I want to see that happen for us both.
I would love to go for a bike ride and not worry about going low (blood glucose levels). Not needing to take extra food with me every time. Not having to check my Dexcom (CGM device) constantly. Just going for a ride for the pure pleasure of riding. I want to experience that. That’s something I want to try.
To learn more about Miguel’s fundraiser, please visit: https://jdrf.akaraisin.com/ui/YourWay2024/p/miguel55
To build your own ‘Diaversary’ fundraising campaign, please visit: https://jdrf.akaraisin.com/ui/YourWay2024/mark-your-diaversary