Here is an overview of our most recent efforts to demand affordable and accessible diabetes technologies for all Canadians living with type 1 diabetes (T1D).
You may remember from our last update that Yukon received #AccessForAll, thanks to the advocacy efforts of adults, parents and others touched by T1D. The Yukon government has moved to fully reimburse continuous glucose monitoring (CGM) and flash glucose monitoring (Flash GM) for people of all ages.
We were also pleased that all the Saskatchewan parties agreed on more coverage. This was great news for those with T1D living in the Yukon and Saskatchewan.
Manitoba
Our advocacy efforts in Manitoba continue to centre around extending age coverage for insulin pumps to 18+ learn more about this issue here.
JDRF is calling for a Made-in-Manitoba plan to support Manitobans in our upcoming budget submission.
In it, we ask that the government remove the current age restrictions for insulin pumps and extend coverage to all ages. We also ask that it invests in public coverage for continuous glucose monitors (CGM) and flash glucose monitors (Flash GM) for all ages. This plan would significantly improve the quality of life and health outcomes for Manitobans with T1D, but also allow for a more equitable and innovative health care system on par with other provinces and territories.
We hope to build on the success from parent and student led advocacy efforts in both the Yukon and Saskatchewan, so that Manitoba doesn’t get left behind.
British Columbia
We hosted four online community events from Jan 26th to Feb 4th that invited members of the BC T1D community and JDRF donors to show their support for #AccessForAll. These events were held to send a clear message to the B. government to cover CGM and Flash GM under B.C. Pharmacare.

The BC government is actively considering coverage for these technologies, and these events were held to ensure that the issue remains front and centre to ensure coverage that those living with type 1 diabetes (T1D) need.
The events were held in Fraser Valley, Northern & Island, the Interior – Tues. Feb 2 and Vancouver Coastal. Healthcare professionals and members of the T1D community shared their stories about the coverage issues and why access to T1D technology is so important. Elected officials were in attendance to connect with and learn from their constituents. We hope that by sending a strong message to BC representatives, we will see a commitment to funding these devices in the next provincial budget.
Pre-Budget recommendations submitted to the Government of Ontario
We are still advocating to the Ontario government to expand device access beyond Flash GM (currently covered for those under age 25, on disability or receiving social assistance who have no private insurance coverage and those over age 65), and also include funding for CGM (Continuous Glucose Monitoring) devices.
Included as well in our pre-budget submission was the recognition of how virtual care has expanded during COVID-19 and is likely to continue once the pandemic ends. Virtual care tied to access to Flash GM and CGM devices reduces both impact on the healthcare system and hallway medicine. This has health and economic benefits for the province.
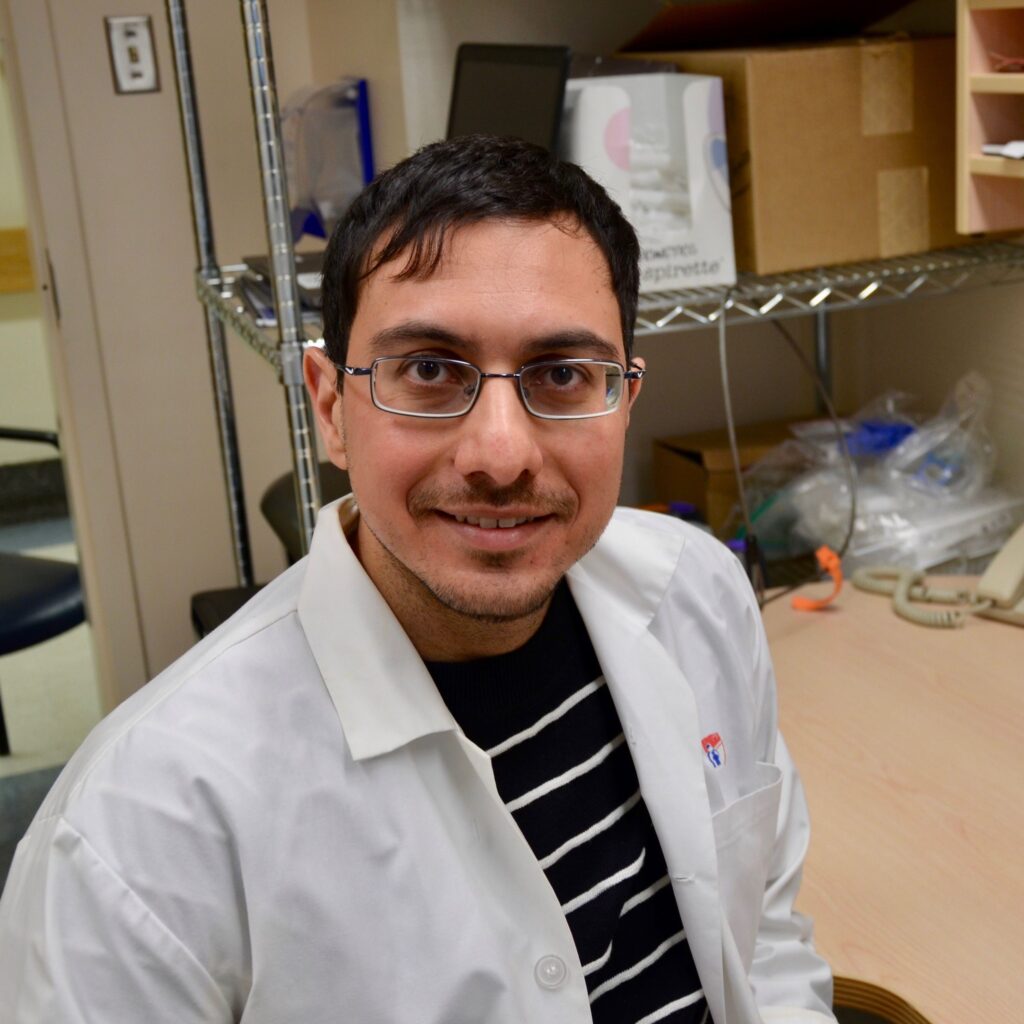
Update from Brooke Roche, MBA, BEDS – Prime Minister’s Youth Council Member
JDRF volunteer advocate Brooks Roche has been extremely busy, reaching out to both members of the PEI and NFLD governments and federal MPs advocating for full coverage of Flash GM, CGM and insulin pumps in Atlantic Canada.
In September, the Prime Minister’s Youth Council met to discuss a wide range of topics with the PM – including the implementation of a national diabetes strategy. Brooks presented a fiscal, social, and celebratory case for comprehensive action, and in response the Prime Minister has committed to advocate in favour of implementing Diabetes 360 and to discuss the matter with Ministers Hajdu and Freeland in their coming meetings. He will also be involved in upcoming discussions with the PM and Minister Qualtrough on the Canada Disability Benefit referenced in the Speech from the Throne.
Brooks is doing amazing advocacy work and we’re very grateful to him.
Read his opinion piece published on CBC News to recognize the milestone anniversary of a 100 years since the discovery of insulin and the call to action for a national diabetes strategy here.
Watch Brooks’ full presentation to PEI Legislative Standing Committee on Health & Social Development
If you’d like to take action, send an email to your provincial representative, requesting accessible and universal CGM and Flash GM coverage today.
Our youth ambassadors took to the Hill virtually in 2020
Our Kids for a Cure Lobby Day-Home Edition was a great success. During the week of November 2nd, delegates joined JDRF for its annual Kids for a Cure Program. This year, due to COVID the event was held virtually.
Kids for a Cure is an initiative designed to raise awareness about the daily challenges faced by those living with type 1 (T1D) diabetes and the need for more Canadian research in this field. Throughout the week, our youth ambassadors share their personal stories of what it is like to live with T1D with Members of Parliament and Senators.
Click here to read some of their stories.
Federal Budget Submission
JDRF’s federal budget submission highlighted the 100th anniversary of the discovery of the insulin hormone– and emphasized how this remains the only treatment for people with diabetes and is not a cure. While technology has greatly improved the lives of people living with T1D, it is now time to more aggressively pursue research into cures.
The following three recommendations were submitted, with supporting evidence both to their demonstrated benefit to the health of Canadians living with T1D and economically.
Recommendation 1: The Government of Canada should honour next year’s centenary of the discovery of insulin through renewed research investment of $15M in the JDRF-CIHR Partnership to Diabetes to be matched by JDRF and its partners.
Recommendation 2: As recommended in the Disability Advisory Committee’s (DAC) First Annual Report, Canadians requiring life-sustaining therapy, including insulin therapy, should automatically qualify for the Disability Tax Credit (DTC). Recommendation 3: As recommended by the Standing Committee on Health in A Diabetes Strategy for Canada, the Government of Canada should invest in the implementation of a national diabetes strategy (Diabetes 360o) with specific outcomes for the different types of diabetes.